The feasibility of high-intensity ESM / EMA in dementia.
TL;DR
Traditionally, people with dementia have been excluded from experience sampling (ESM) / ecological momentary assessment (EMA) studies due to assumptions about their poor digital skills and cognitive challenges. A new study led by Dr. Laura Dewitte and co-authored by the m-Path team, shows this is changing: with a co-designed study design, an intensive smartphone-based ESM / EMA approach proved not only feasible, but also meaningful. Participants reported high engagement, low burden, and even enjoyment, while delivering rich first-person data on their daily lives.
Traditionally, researchers have assumed that people with dementia can’t participate in digital self-report studies. The reasoning? Older adults might be less familiar with technology, and cognitive difficulties could make it too hard to reflect on feelings or complete repeated questionnaires.
Because of these assumptions, most studies have relied on passive sensing data (like movement or sleep patterns) or caregiver reports rather than asking people with dementia directly. But this misses something essential: their own voice in describing their inner world and lived experiences.
Testing the feasiblity of an intensive ESM / EMA approach
In this study, 12 people with young-onset dementia (ages 52–72) participated in a 10-day, high-frequency smartphone-based ESM protocol using our m-Path app.
- Seven momentary surveys captured momentary mood and thoughts.
- An evening survey asked about life satisfaction and meaning.
- A voice recording option let participants simply speak their thoughts instead of typing, reducing burden and capturing richer, more natural data.
This intensive setup (usually seen as too demanding for dementia populations) turned out to be both manageable and insightful.
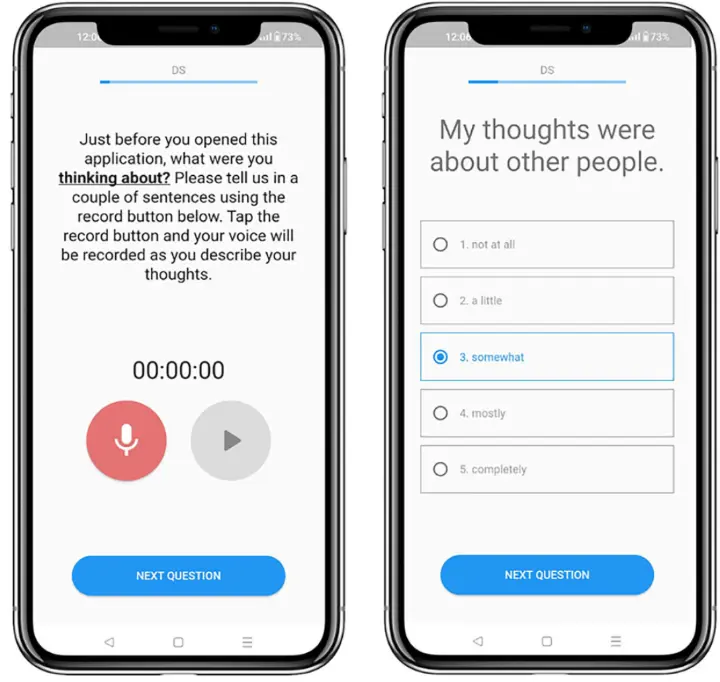
m-Path screenhots that demonstrate the voice recording item and simplified Likert questions.
Check out our dedicated manual page to learn how to add the voice recording item to your study!
Co-design with stakeholders
A key ingredient for succesful implementation was stakeholder consultation. Before launching the study, researchers worked with a Dementia Lived Experience Expert Advisory Panel. Their feedback shaped the protocol in important ways, including:
- Replacing slider scales with clickable Likert scales for easier interaction.
- Adding a training video alongside written instructions.
- Extending the data collection from 7 to 10 days to better capture variability.
- Recruiting a broad, transdiagnostic sample for inclusivity.
This co-design process didn’t just improve feasibility, it also ensured that participants felt the study was made for them, not imposed on them.
What we found
1. Strong participation.
Over half of those invited joined, which is higher than many dementia and even general population ESM studies. No one dropped out.
2. High compliance.
Participants completed 80% of all prompts, despite the high frequency. Surveys took just 2 minutes on average.
3. Positive user experiences.
In the participation evaluation, people reported low burden, high motivation, and satisfaction with the support they received. Several said they appreciated the chance to reflect on their daily thoughts and feelings.
4. Sufficient variability in the momentary data.
The data showed plenty of within-person variation in mood, thoughts, and meaning, exactly what ESM / EMA is designed to capture.
Why this matters for your research
This study directly challenges the idea that people with dementia can’t engage with high-intensity digital research, an incorrect assumption that is also often held about other difficult-to-reach study populations (e.g., clinical samples in high distress, young children or elderly, people with intellectual disabilities, etc.). With the right adaptations and support, we believe that everyone can successfully participate in an ESM / EMA study.
Practical take-aways
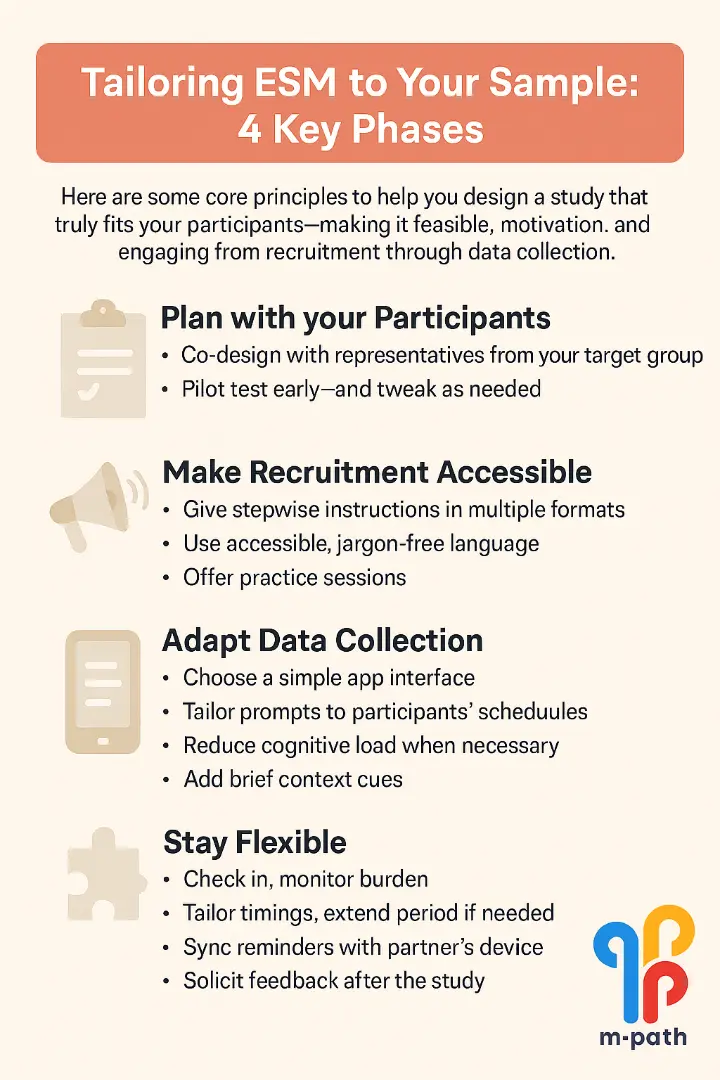
In this cheat sheet, we provide some core principles to help you design a study that truly fits your participants, making it feasible, motivating, and engaging from recruitment through data collection.
👉 Explore the full (open-access) paper here: npj Dementia, 2025.
